Emerging COVID-19 success story: Vietnam’s commitment to containment
As of December 31, 2020, Vietnam had reported 1,465 laboratory confirmed cases of COVID-19 and 35 deaths.2 This success has been attributed to several key factors, including a well-developed public health system, a decisive central government, and a proactive containment strategy based on comprehensive testing, tracing, and quarantining.
Detect: Vietnam has taken a targeted approach to testing, scaling it up in areas with community transmission. Contact tracing is comprehensive, with three degrees of contacts traced for each positive case.
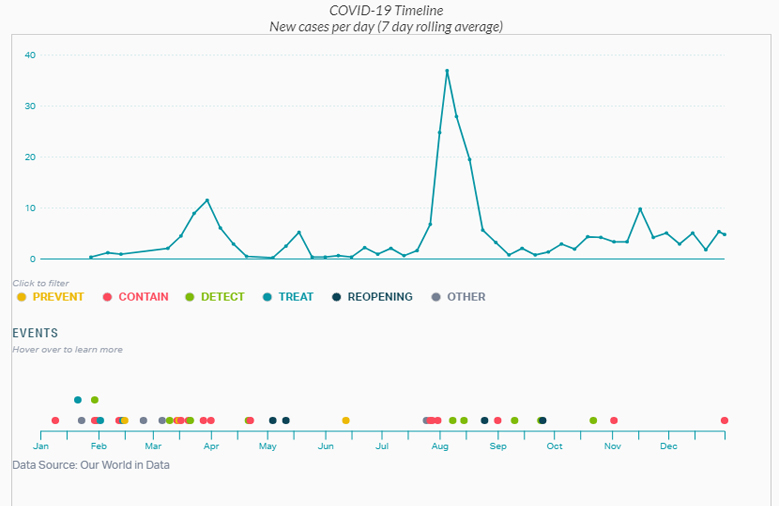
Contain: As a result of its detection process, hundreds of thousands of people, including international travelers and those who had close contact with people who tested positive, were placed in quarantine centers run by the government, greatly reducing both household and community transmission. Hot spots with demonstrated community transmission, including Da Nang during its outbreak in July and August 2020, were locked down immediately, and the government communicated frequently with citizens to keep them informed and involved in the public health response.
One of the reasons Vietnam was able to act so quickly and keep the case count so low is that the country experienced a severe acute respiratory syndrome (SARS) epidemic in 2003 and human cases of avian influenza between 2004 and 2010. As a result, Vietnam had both the experience and infrastructure to take appropriate action. Vietnam makes many key containment decisions in a matter of days, which may take weeks for governments in other countries to make. Although Vietnam is a highly centralized country, a number of key decisions were made at the local level, which also contributed to the swift response.
Country Overview
Since the 1980s, Vietnam, a country of nearly 100 million people, has undergone a significant economic transformation. The adoption of economic reforms known as the Doi Moi policies in the mid-1980s turned a centrally planned economy into a socialist-oriented market economy, setting Vietnam on a path to its current middle-income status.
Vietnam has invested heavily in its health care system, with public health expenditures per capita increasing an average rate of 9 percent per year between 2000 and 2016.3 These investments have paid off with rapidly improving health indicators. For example, infant mortality and maternal mortality decreased by more than half between 1990 and 2018.4
Vietnam has a history of successfully managing pandemics: it was the second country after China to face SARS and, after 63 cases and five deaths, it was the first country declared SARS-free by the World Health Organization (WHO).5 Many interventions pioneered by Vietnam during the SARS epidemic are being used to respond to COVID-19. Similarly, its experience with epidemic preparedness and response measures may have led to greater willingness among people in the country to comply with a central public health response.
In the wake of the SARS epidemic, Vietnam increased investments in its public health infrastructure, developing a national public health emergency operations center and a national public health surveillance system.6 The national center and four regional centers run exercises and trainings to prepare key stakeholders in government for outbreaks, and they have managed preparedness and response efforts for measles, Ebola, Middle East respiratory syndrome (MERS), and Zika. Throughout the COVID-19 pandemic, the government has continued to incorporate new lessons and regularly conducts intra-action and after-action reviews.7
Vietnam has long maintained robust systems to collect and aggregate public data, and in 2009 it shifted to a nearly real-time, web-based system. Since 2016, hospitals are required to report notifiable diseases within 24 hours to a central database, ensuring that the Ministry of Health can track epidemiological developments across the country.8 In collaboration with the US Centers for Disease Control and Prevention (CDC), Vietnam implemented an innovative “event-based” surveillance program in 2018. Event-based surveillance empowers members of the public, including teachers, pharmacists, religious leaders, and even traditional medicine healers, to report public health events. The goal is to identify clusters of people who have similar symptoms that might suggest an outbreak is emerging.9